Digital Health Investment Trends
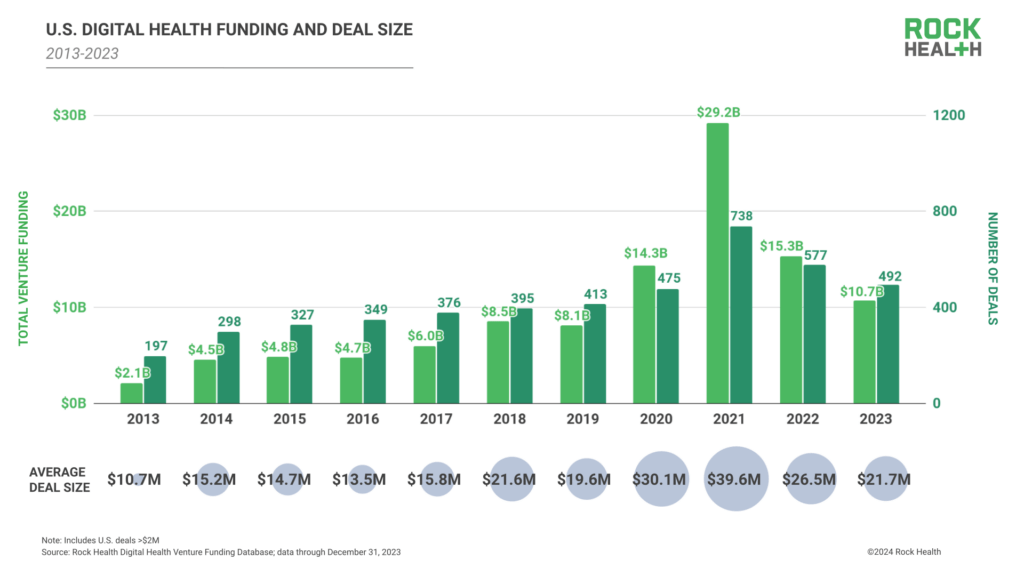
This chart from Rock Health perfectly illustrates the trajectory of the digital health industry since the COVID-19 pandemic began in March 2020. Between 2015 and 2019, the average annual investment in U.S. digital health companies was $6.4 billion. In 2020, that number more than doubled to $14.8 billion, and in 2021, it doubled again to $29.2 billion. The industry cooled off in 2022, with funding falling back to the 2020 level of $15.3 billion (a 50% decline), and 2023 funding dropped another 33% to $10.7 billion.
While much is made of the decline in digital healthcare investment since its peak in 2021, the $10.7 billion invested in 2023 is still approximately 40% higher than the average deal size in the five years prior to COVID. Additionally, the average deal size in 2023 ($21.7 million) was higher than the highest pre-pandemic peak ($21.6 million in 2018).
In short, the rumors of the digital health industry’s demise are somewhat exaggerated. If the investment numbers weren’t enough evidence, the attendees at this year’s AHIP conference certainly were.
AHIP stands for America’s Health Insurance Plans, the national trade association representing the U.S. health insurance industry. Every year, AHIP holds its signature industry conference in June, focusing on the private health insurance market. This includes large and small group health insurance, as well as Medicare Advantage and individual health insurance products – some of the most commonly used health insurance options in the country.
AI Takes Center Stage at AHIP 2024
This year’s AHIP conference was held in Las Vegas. With the economic slowdown in 2024, I expected lower attendance and fewer vendors.
I was wrong.
The AHIP exhibit floor resembled an NVIDIA shareholders meeting, buzzing with excitement about the transformative potential of Artificial Intelligence (AI) in healthcare. From care navigation to chronic disease management, the exhibit hall and private meeting rooms showcased a vibrant ecosystem of companies, all touting their ability to leverage AI to improve patient outcomes and drive healthcare efficiency.
During my time at the show, I spoke with executives from fourteen companies including Kaia Health, PreventScripts, The Helper Bees, Decision Point by mPulse, Evernorth Health Services, PatientGenie, Sutherland Healthcare Solutions, Sidekick Health, Color Health, Navitus Health Solutions, Fair Square Medicare, Homebrew Health, Radiant Graph and Writer.
Of these, 57% leveraged AI. Here’s a quick summary of them:
- PreventScripts uses AI to identify at-risk patients, deliver care plans, and improve behaviors;
- Decision Point by mPulse uses AI to help their clients understand and predict their member’s journey through the health system and enables sustained improvements in member health outcomes;
- PatientGenie uses Large Language Models (LLMs) and a “patented data engine” to assists patients in navigating provider searches;
- Sidekick Health uses AI to empower patients by digitizing their healthcare access;
- Fair Square Medicare does AI-driven health plan navigation;
- Homebrew Health is building an AI-driven care navigation platform;
- Radiant Graph has an AI-driven member segmentation, personalization & engagement platform
- Writer boasts a full-stack generative AI for healthcare.
We’ll talk to some of these companies this year on Charting a New Course, but, suffice-it-to-say, that’s a lot of AI.
AI & Charting a New Course Season 2
As a corporate executive in charge of growth marketing and lead-generation, I’ve spent the last four years spending 10 to 15% of investor’s money trying to drive patients to use digital health products through direct-to-consumer marketing.
While I’m proud of the growth my teams have been able to drive through channels like Meta, Google, Tatari, Reddit, YouTube, LinkedIn and others, those are not the channels consumers use to find healthcare. In fact, what I’ve found through surveys and partnerships is that most consumers in search of treatment start by going to their health plan’s website.
For example, at Bicycle Health we partner with Kyruus Health (https://kyruushealth.com/) to reach patients when they check in for doctor visits, and when they search for treatment through their insurer’s website.
What was fascinating to learn through that partnership was that the volume of patients searching for opioid use disorder (OUD) treatment through a health plan search tool was roughly equivalent to the volume of keyword searches we were paying for on Google (once we adjusted for Kyruus’ market share and the states where we provided treatment).
Said another way, if health plan search tools worked as well as Google at surfacing treatment providers who were in network, digital health point solutions could spend less money on direct to consumer marketing and more on their core business function, which is to deliver high-quality care at a lower cost.
This waste of resources is, frankly, why I wanted to start season 2 of Charting a New Course by highlighting companies focused on care navigation and collaboration, like Auxa Health, Endear Health, Socially Determined, Unite Us, Dina Care, The Helper Bees, CarePort Health, naviHealth, 9am.health, Cecelia Health, HabitNu, Omada Health, Rimidi Health, PreventScripts, Babyscripts, amd Glooko.
My enthusiasm for this group of companies centered around my frustration with the existing healthcare ecosystem that makes it so hard for patients to find the care they need that is covered by their health insurance.
A nod to Value-Based Care
It’s customary for AHIP to dedicate time to value-based care (VBC). The promise of value-based care was to flip the script on traditional healthcare by prioritizing patient outcomes and quality of care over the quantity of services rendered. Unlike fee-for-service models that reward the number of procedures performed, value-based care focuses on delivering the best possible health outcomes at a reasonable cost.
The goal of VBC is to emphasize preventive care to promote healthy behaviors that reduce chronic conditions and help manage those with chronic illnesses more effectively to prevent complications, through better coordination across a team of providers.
However, the challenges with VBC persist. In healthcare, it’s not easy to define and measure “value,” and adapting traditional financial models, and ensuring secure data sharing across providers for effective care coordination, also present challenges.
I don’t mean to belittle the space, because I wholly support the concept, but every year we see costs go up as health conditions worsen while we wait for VBC to deliver on its promise and potential.
Even so, I love the companies that continue to press ahead in this space. In particular, I enjoyed my conversations with representatives at the following companies who continue to chase the dream.
Interesting Companies Shaping the VBC Landscape
- The Helper Bees: This company challenges care.com by providing a curated network of rigorously vetted in-home care providers, focusing on quality and high standards. They act as an e-commerce platform for qualified care services, alleviating the burden of vetting providers for patients and families.
- Evernorth Health Services: Evernorth offers at-home primary and post-acute care services, aiming to improve patient convenience and outcomes.
- Color Health: This company excels in virtual at-home cancer screening, aiming to improve early detection and accessibility.
- Kaia Health: Kaia offers digital interventions specifically for chronic health issues, providing patients with convenient and effective management tools.
A Final Note on Exhibitors
The conference reaffirmed the immense potential of AI in healthcare. As we navigate this exciting yet complex landscape, maintaining a critical perspective alongside a passion for innovation is vital. By fostering collaboration and prioritizing equitable access, we can leverage the power of AI to transform healthcare delivery for the betterment of all.
On Keynotes: It’s For AHIP to Revive the Brawl
I’ve been going to AHIP conferences since 2009. Back in the good ol’ days, circa 2011, when the Affordable Care Act was a political piñata getting whacked from both sides. To AHIP’s credit, they brought in James Carville and Mary Matalin for a good old-fashioned partisan brawl. It wasn’t polite, but it was productive and it was honest.
Fast forward to 2024. AHIP’s big idea for “restoring faith in healthcare” was a quasi-kumbaya session between Scott Jennings and Van Jones. Don’t get me wrong, these guys did a fine job there was no fire or passion, and there was really no politics.
Today in America, more people identify as independents (43%) than those who identify as Democrats (27%) or Republicans (also 27%). It should come as no surprise then that RJK Jr., the independent candidate for president is getting 15 percent of the vote nationally and winning among people under age 30 and among independents. And, by the way, he’s not a big fan of our healthcare industry.
As an industry, we need to embrace the fact that COVID-19 vaccine mandates deeply divided this country. In the middle of a presidential election, with three candidates getting at least 15 percent of the vote who can’t agree on the impact of COVID and its vaccines, AHIP attendees deserved an open, honest discussion between these leaders, even if it was destined to become a brawl.
Trust in the healthcare system is at an all time low, and people are asking serious questions about the influence of industry in their healthcare. AHIP should be demanding that the leaders of each party attend their conference for thoughtful, measured, and honest conversation about their visions for our path forward.
The dirty secret we have to acknowledge is trust is shot. It’s hard to listen to a presidential candidate like RFK Jr, or to read the arguments of Attorney Generals in states like Kansas and Indiana and not have serious questions about the trustworthiness of some of our institutions.
The pharmaceutical industry’s track record is enough, on its own, to warrant serious concerns. From opioids to talcum powder to vaccines, we’ve seen these companies for decades put products on the market that at best were misrepresented and at worst were knowingly harmful.
To act as if people were buying into conspiracy theories simply because they had mistrust in some of these companies is, in my opinion, the worst kind of gaslighting.
So, what’s the answer? I’d like AHIP to take a page out of its own ACA playbook, ditch the polite panels, and foster real debate. Invite the candidates, or their surrogates to have it out. I believe the only way to stop “misinformation” is with open dialog and debate. Silencing dissent never leads to good things.
AI’s on the horizon, and healthcare’s about to get a whole lot more complex. I’d love to see AHIP get comfortable with messy, controversial and even downright ugly topics.




Leave a comment